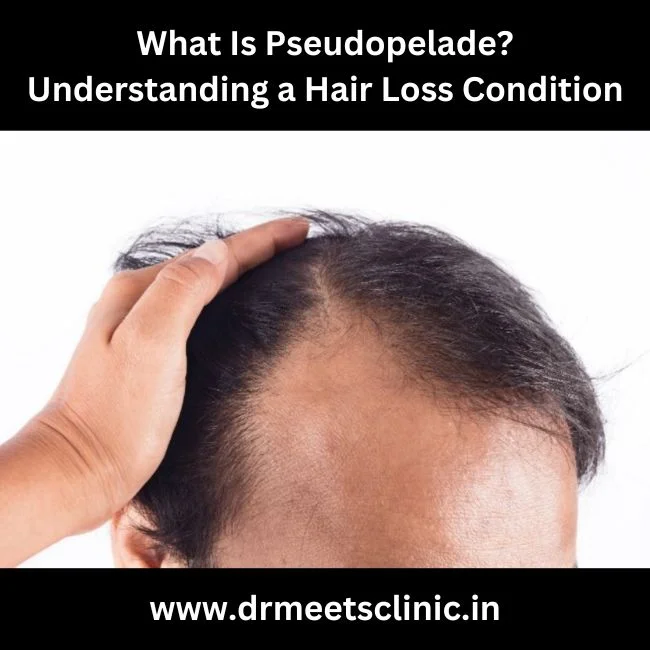
What Is Pseudopelade?
Pseudopelade, also known as pseudopelade of Brocq, is a rare, chronic form of hair loss that primarily affects the scalp. It is classified under a group of conditions known as scarring alopecia or cicatricial alopecia. In this condition, hair follicles are permanently destroyed, leading to irreversible hair loss in the affected areas. The scalp in these regions becomes smooth, shiny, and devoid of hair, with the skin often appearing scarred.
Unlike other hair loss conditions, pseudopelade is generally non-inflammatory and asymptomatic, meaning there is little to no itching, pain, or redness associated with it. This lack of symptoms can make it difficult to diagnose early, as individuals may not seek medical help until significant hair loss has occurred.
Causes and Risk Factors
Other potential factors that may contribute to the development of pseudopelade include:
Signs and Symptoms of Pseudopelade
Key characteristics of pseudopelade include:
Diagnosis of Pseudopelade
Diagnosing pseudopelade can be challenging, as it shares similarities with other forms of scarring alopecia and hair loss conditions. Dermatologists and trichologists use several diagnostic methods to identify pseudopelade, including:
Clinical examination: A thorough examination of the scalp is the first step. The dermatologist looks for characteristic signs of pseudopelade, such as the smooth, shiny patches of hair loss and the “footprint in the snow” pattern.
Treatment Options for Pseudopelade
Unfortunately, once pseudopelade has destroyed the hair follicles, the hair loss is permanent. However, early diagnosis and intervention can slow or halt the progression of the condition, preventing further hair loss. Treatment options focus on managing the underlying causes and reducing inflammation, if present.
Topical corticosteroids: If there is evidence of active inflammation, corticosteroids may be prescribed to reduce immune system activity and slow the progression of the disease.
Living with Pseudopelade
For individuals dealing with pseudopelade, maintaining a healthy scalp, managing stress, and consulting with a dermatologist regularly are key steps in slowing the progression of the disease. Wearing wigs, hairpieces, or opting for scalp micropigmentation can also help improve the appearance of the scalp and enhance confidence.
Conclusion
A rare and complicated hair loss disorder called pseudopelade has the potential to cause lifelong baldness. Although the exact causes are still not fully understood, early detection and intervention can prevent extensive hair loss. Consulting with a dermatologist or hair loss specialist is crucial for managing the condition and exploring treatment options that can slow its progression. For those experiencing unexplained hair loss, understanding pseudopelade can be the first step towards finding effective solutions and coping with this challenging condition.